Cutting-Edge Research
neuroscience
Forging a New Path to Treat Autism
by Matthew Hutson
Recognizing a face. Riding a bike. Reading a book. Without long-term memory, none of these tasks tasks would be possible. Neuroscientists have long aimed to explain the intricate molecular clockwork that allows experience to accumulate so that we may tackle each day more capably than the last. A malfunction in any one cog can leave us forgetful or, as NYU researchers have found, not forgetful enough. Their work, published recently in Neuron, reveals new information about one of the enzymes crucial to long-term memory and may soon lead to novel treatments for neurological disorders, such as autism and obsessive compulsive disorder, or OCD.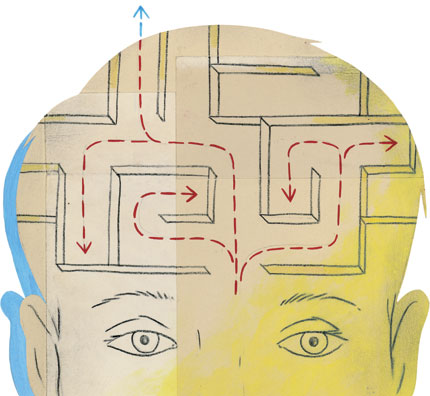
Long-term memory is thought to rely on a process called long-term potentiation, where, when two neurons fire together, their synaptic connection is altered to let them communicate more easily. As we learn, certain connections are strengthened more than others, etching pathways in the networks of our brains. This requires the synthesis of new proteins, and neuroscientist Eric Klann, along with collaborators at NYU and the Baylor College of Medicine in Houston, found some surprising things about one of the enzymes critical to the process.
The researchers developed mice lacking FKBP12, a protein that interferes with the enzyme in question, mTOR, which regulates the cellular manufacture of other proteins. Removing FKBP12 should let mTOR do its thing unchecked, facilitating long-term potentiation. “In our original tests, it looked like there was enhanced memory,” Klann says, “but then we found it was a little more complicated. Although the mice could memorize things—in some cases better than normal mice—they weren’t flexible.” The mice could learn a maze without a hitch, but if you put them in a slightly different maze, they hit a dead end. They couldn’t adjust to changing conditions.
Further tests revealed that these affected mice showed behavior resembling that of humans with autism and OCD. For example, they repeatedly buried marbles, a pattern similar to tics in autism or constant hand-washing in OCD. When presented with a previously seen object and a novel one, the mice showed more interest in the old object, revealing discomfort with the unfamiliar. And when given a shock in one environment, they were more likely than normal mice to freeze when placed back in that environment. “If something bad happens at school,” Klann says, “some autistic children have a difficult time going back because they’re fearful.” The memory is too persistent.
Both biochemical and neurophysiological experiments confirmed the source of the repetitive behavior. Removal of FKBP12 did indeed enhance the activity of the mTOR enzyme, and scientists found increased mTOR signaling in several areas of the mouse brains. Klann’s team is now trying to isolate which molecules downstream of mTOR’s enyzmatic activity are responsible for its effects on memory. Then maybe they can pharmacologically target those pieces of the clockwork.
Importantly, the changes in the mice did not kick in until two or three weeks after birth, implying that autism and related disorders can develop even in people who are born healthy. “It’s not necessarily the case that the brain is wired differently,” Klann says. “It also could be that these pathways are just misregulated.” While correcting the misregulation may be too tall an order, Klann hopes that some of the symptoms that decrease the quality of life, such as repetitive behaviors, could be treated—even in an adult. Such a breakthrough, he believes, is “not far off at all.”
parasitology
Cracking Malaria’s Code
by Lindsay Mueller / CAS ’09

Plasmodium vivax is not the type of malaria parasite that kills you, explains parasitologist Jane Carlton, “but they say it makes you wish you were dead.” It causes flu-like symptoms—aches, shivers, high temperature, and a general feeling of malaise—and is responsible for more than a quarter of the 515 million malaria cases diagnosed worldwide each year. If infected, a patient might feel fine one day and ill the next. “The danger is that you can have it and not even know it because the parasite can hibernate in the liver and remain dormant for months, even years,” Carlton says.
So many will take heart in knowing that Carlton and a team of colleagues at the NYU School of Medicine have decoded the DNA for this species, which is endemic in Asia and the Americas. Their work, published as the cover story in a recent issue of the journal Nature, will allow them to identify weak spots in the parasite’s armor and, most important, provide a foundation for the development of a vaccine.
Carlton’s discovery marks a milestone in malaria research. It is impossible to grow the parasite in a culture, mainly because it requires young red blood cells, which are notoriously difficult to cultivate. Carlton and her team partnered with the Centers for Disease Control and Prevention to infect several South American squirrel monkeys with an El Salvadorian strain of P. vivax in order to obtain sufficient DNA for the project.
In the future, Carlton and her team plan to collect blood samples from P. vivax-infected patients all over the world to better understand different strains of the disease and, in time, target treatments for it.
dentistry
Mouth Reveals an Alzheimer’s Clue
by Ted Boscia
For most people, the nightly ritual of brushing, flossing, gargling, and rinsing is ingrained at a young age in the hopes of keeping their teeth sparkling white and armed against decay. But a new study suggests that these simple acts, which take just a few minutes each day, might also help stave off one of the most devastating diseases of the brain.
A team of NYU doctors recently linked Alzheimer’s disease to gum disease, the latest discovery in a growing body of evidence tying bacterial infections that elevate inflammatory molecules in the brain to Alzheimer’s, which more than five million Americans suffer from. Earlier research at the University of British Columbia showed that those suffering from dementia also had high levels of the bacterium found in periodontal disease.
“I can’t state that the management of periodontal disease would suddenly or immediately halt Alzheimer’s,” cautions Angela Kamer, assistant professor at the College of Dentistry, and leader of the NYU study. “But it could slow its progression and also warn doctors and patients to be more aware of the risk.”
Kamer and her team compared 18 patients with early signs of Alzheimer’s to 16 patients with normal brain function and discovered a sharp difference. While 72 percent of the Alzheimer’s patients displayed an antibody associated with periodontal bacteria, only 38 percent did in the other group.
Kamer recently presented her findings at the Alzheimer’s Association’s International Conference in Chicago. While the work may lead dentists to screen their patients more actively for periodontal disease, it could also help scientists more precisely identify the causes of Alzheimer’s and shape the search for more effective treatments, or even a cure. Already, brain specialist Mony de Leon, director of the NYU Center for Brain Health, has integrated Kamer’s findings into his hunt for biological markers for the disease.
illustration © Leigh Wells; Photo © 2009 Photo Researchers, Inc.







